Patient Services
Posture is Life: Influencing Longevity through Postural Correction
The Posture Connection
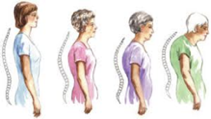
Posture has become one of the most overlooked aspects of good health and longevity. Research has shown a clear and direct connection between poor posture and diminished quality and longevity of human life. Spinal pain, headache, mood, blood pressure, pulse and lung capacity are among the functions most easily influenced by posture.

“You are only as young as your spine.”
-Jack LaLanne, DC
As the head moves forward all measures of health status are significantly reduced.
Rene Cailliet, Director of the Department of Physical Medicine and Rehabilitation, University of Southern California, concluded that forward head posture can add up to thirty pounds of abnormal leverage on the spine, and can reduce lung capacity by as much as 30%, which can lead to heart and blood vascular disease. He determined a relationship between forward head posture and the digestive system, as well as endorphin production affecting pain and the experience of pain.
According to Kapandji, Physiology of the Joints, Volume III: For every inch that the head moves forward in posture, it increases the weight of the head on the neck by 10 pounds. For example, a forward posture of 3 inches increases the weight of the head on the neck by 30 pounds and the pressure put on the muscles increases 6 times.

The British Regional Heart Study
As a part of the British Regional Heart Study, scientists found that men who lost 3cm in height were 64% more likely to die of a heart attack than those who lost less than 1cm and that over the 20-year period of the study, men lost an average of 1.67cm. That height loss was associated with a 42% increased risk of heart attacks, even in men who had no history of cardiovascular disease.

Our Posture = Our Emotional State
We can tell a lot about a person from the way they carry themselves. For instance, picture the way someone stands when they are feeling depressed: mid-back and shoulders rolled forward, head hanging, gaze focused on the ground. Not exactly the picture of health.
Yoga gurus have long said that it is impossible to be depressed with your armpits open.

Posture and Life Expectancy
A group of scientists led by Dr. Deborah M. Kado wanted to see if there was any correlation between postural distortion and a person’s health. They started with the biggest health problem: death. They asked: “Was there any correlation between a person having a hyperkyphosis and having a decreased life expectancy?”
The Frightening Long-Term Effects
Dr. Kado reported in the Journal of the American Geriatrics Society that persons with hyperkyphosis (hunched over – head and shoulders rolled forward) were two times more likely to die from pulmonary causes. They were also 2.4 times more likely to die from cardiovascular disease than those without poor posture
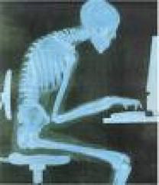
Too Much Sitting Can Shorten Your Life
According to a study from the American Cancer Society, the amount of time you spend sitting can affect your risk of death. Prolonged periods of sitting have a negative influence on key metabolic factors like triglycerides, high-density lipoprotein, cholesterol, and a number of other biomarkers of obesity and other chronic diseases.
To live a long, active, energetic life, few things matter more than posture.

This quote by Thomas Meyers, Author of Anatomy Trains, says it all… “Movement becomes a habit, which becomes posture, which becomes structure.”

Postural Assessment is Key
Postural assessment and correction is the key in the majority of non-traumatic neck pain. It’s not uncommon to observe 2″ of anterior head placement in new patients. Would you be surprised that your neck and shoulders hurt if you had a 12 pound bowling ball hanging around your neck?

What is Ergonomics?
The scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, methods and data to design in order to optimize human well-being and overall system performance.
Ergonomics means: “fitting the job to the worker” from the Greek, Ergo = Work and Nomos = Laws
What are Work-Related Musculoskeletal Disorders (WMSD)?
- WMSDs are soft tissue injuries which occur gradually, also known as:
- Cumulative Trauma Disorders (CTDs)
- Repetitive Strain Injuries (RSIs)
- Overuse injuries
What are Ergonomic Conditions?
Disorders of the soft tissue – specifically: Muscles, nerves, tendons, ligaments, joints, cartilage, blood vessels, spinal discs.
What Are Some of the Symptoms of WMSDs? Discomfort, pain, numbness, tingling, inflammation, burning, swelling, change in color, tightness, loss of flexibility, discomfort, pain, numbness.
What Can Cause Symptoms of WMSDs? Heavy, frequent or awkward lifting, pushing, pulling or carrying loads, working in awkward postures, hand intensive work, vibration, contact stress.
Risk of injury depends upon: duration of exposure, frequency of exposure, intensity of exposure, or a combinations of risk factors.
Risk factors for maximum lifting: There are only recommendations for the maximum weight a person can lift.
Frequent lifting: A little more than twice per minute.
Awkward lifting: Lifting above the shoulders, below the knees, or at arm’s length. Lifting above the shoulders, below the knees, or at arm’s length.
Risk Factors for WMSDs: Awkward Postures are squatting, kneeling, bending.
Reducing Low Work: Raise and/or tilt the work for better access, use a stool for ground level work, use tools with longer handles, alternate between bending, kneeling, sitting and squatting.
Reducing Reaching: Keep items within close reach, design reach distance for the shortest worker, , emove obstacles, use gravity feed racks.
Risk Factors for WMSDs: Hand Intensive Work
Hand Intensive Work: Highly Repetitive Work
Making the same motion repeatedly can cause a lot of wear and tear on the joints being used, and if you don’t rest to allow time for them to heal, the damage can just keep building up.
Reducing Repetition: Arrange work to avoid unnecessary motions, let power tools and machinery do the work, spread repetitive work out during the day, take stretch pauses, rotate task with co-workers if possible, change hands or motions frequently.
Your grip strength decreases when you: bend your wrists, pick up slippery items, wear poorly fitting gloves, have cold hands.
Recognition and Reporting Signs and Symptoms
Report signs or symptoms if:
- Pain is persistent, severe or worsening
- Pain radiates
- Symptoms include numbness or tingling
- Symptoms keep you from sleeping at night
- Fingers blanch or turn white
Why Is It Important to Report Signs and Symptoms Early? Acute injuries can easily become chronic injuries and can sometimes lead to disability, even surgery. Early treatment save time and money. It’s important for your own health to report symptoms as early as you can.
Getting Involved! Look at your job, come up with solutions, work with solutions. Take part in training. Take responsibility for changing the way you do your job. Help to make sure efforts are successful!
5 Key Points to Remember:
- Ergonomics can help you on your job
- WMSDs can happen in jobs with risk factors
- Risk factors can be reduced and WMSDs prevented
- Reporting signs and symptoms early is important
- You can help your company put ergonomics changes into place
What is Chiropractic
Chiropractic is a health care profession that focuses on treatment of disorders within the musculoskeletal and nervous systems. Muscular, nervous, and skeletal problems are among the symptoms treated by chiropractic care.
Chiropractors specialize in correcting spinal misalignment. These misalignments of the spine are called subluxations. Often chiropractors manipulate the spine and various parts of the body by hand using specific procedures. Chiropractors also use conventional diagnostic tests such as MRIs, X-Rays, and lab work to provide treatment for their patients. Chiropractic treatment may also include:
- Electrotherapy
- Ice/heat therapy
- Therapeutic exercise
- Therapeutic ultrasound
- Lifestyle counseling
- Massage therapy
- Nutritional counseling
- Physical rehabilitation
- Stress management
Heat Therapy
Most commonly used for rehabilitation purposes, heat therapy is the application of heat to the body for pain relief and health. It can be performed using something as simple as a heat to cloth to as advanced as ultrasound.
The therapeutic effects of heat include increasing the extensibility of collagen tissues; decreasing joint stiffness; reducing pain; relieving muscle spasms; reducing inflammation, edema, and aids in the post acute phase of healing; and increasing blood flow. The increased blood flow to the affected area provides proteins, nutrients, and oxygen for better healing.
Heat creates higher tissue temperatures, which produces vasodilation that increases the supply of oxygen, and nutrients and the elimination of carbon dioxide and metabolic waste. It is useful for muscle spasms, myalgia, fibromyalgia, contracture, and bursitis.Heat therapy can also be used for the treatment of headaches and migraines.
Heat therapy is only part of the therapeutic procedure that is chiropractic, and rarely provides a full extent of recovery without it.
Heat therapy should not be used on swollen or bruised tissues. It is advised that patients who have dermatitis, deep vein thrombosis, diabetes, peripheral vascular disease, open wounds, and cardiovascular conditions such as hypertension not use heat therapy.
Adjustments
Chiropractic adjustment can only be applied to joints in the spine and correction of misalignment or subluxation that may occur in that area. 95 percent of all spinal adjustments in the world are performed by chiropractors. Chiropractic adjustment frees the vertebrae to adjust to its natural position. The natural state of the body knows how to correct itself once it is free to do so with the help of chiropractic adjustment.
Chiropractic adjustments can help prevent and treat many conditions such as the following:
- Arthritis
- Bursitis
- Carpal tunnel syndrome and other repetitive strain disorders
- Chronic muscle pain and stiffness
- Headaches
- Most musculoskeletal and sports-related injuries
- Nerve disorders
- Pain and stiffness in the back, chest, abdomen, neck, hips and shoulders, as well as extremities, such as arms, legs, and feet
- Sciatica pain
- Scoliosis
- Tendonitis
- Whiplash and other traumatic injuries
Some common adjustment methods include:
- Toggle Drop: This is when the chiropractor, using crossed hands, presses down firmly on a particular area of the spine. Then, with a quick and precise thrust, the chiropractor adjusts the spine. This is done to improve mobility in the vertebral joints.
- Lumbar Roll (aka side posture): The chiropractor positions the patient on his or her side, then applies a quick and precise manipulative thrust to the misaligned vertebra, returning it to its proper position.
- Release Work: The chiropractor applies gentle pressure using his or her fingertips to separate the vertebrae.
- Table adjustments: The patient lies on a special table with sections that drop down. The chiropractor applies a quick thrust at the same time the section drops. The dropping of the table allows for a lighter adjustment without the twisting positions that can accompany other techniques.
- Instrument adjustments: Often the gentlest methods of adjusting the spine. The patient lies on the table face down while the chiropractor uses a spring-loaded activator instrument to perform the adjustment. This technique is often used to perform adjustments on animals as well.
- Manipulation under anesthesia (MUA): This is performed by a chiropractor certified in this technique in a hospital outpatient setting when the patient is unresponsive to traditional adjustments.Chiropractors take many factors—including size, weight, and muscle structure—into consideration when deciding on which adjustment to make. Sometimes, ice, electrical stimulation, or massage therapy (including traction massage) are used prior to a spinal manipulation in order to relax the muscles.
Patients with chronic pain my require anesthesia during their treatment. This procedure is safe and only reserved for patients with special circumstance. Chiropractic adjustments, when performed by a skillful professional, are significantly safe methods of spinal correction.
Craniosacral therapy (CST) is a form of bodywork that is focused primarily on the concept of primary respiration and regulating the flow of cerebrospinal fluid by using therapeutic touch to manipulate the synarthrodial joints of the cranium. This procedure is proven to often relieve symptoms of stress and tension.
The following are observed benefits from chiropractic adjustments:
- Increased blood flow
- Increased body secretion of melatonin and endorphins
- Increased pain tolerance levels
- Increased range of motion
- Reduced blood pressure
- Reduced tension
- Reduced muscle pain
Popping sounds heard during a chiropractic adjustments are usually caused by pockets of air being released from behind the joints. Mild aching or soreness may be present after a chiropractic visit, but is typically gone shortly after and easily relieved with the application of ice or heat.
Benefits of Chiropractic Care
The alignment of vertebrae in your spine can be the determining factor in a number of health symptoms that affect our overall body of health. This implied presence of an incomplete or partial dislocation of a joint is called a subluxation. Joint mobility can be restored through massage and carefully applied pressure which will allow your body reach homeostasis, its natural state of balance. Nerve energy is restored to its normal flow when the joints in your spine are allowed to return to their proper positions and your body is able to return to its natural healing process.
While Chiropractic care is mostly known for its assistance in relieving pain in your joints, patients of chiropractic care have also reported that their treatment resulted in significant relief from all of the following as well: headaches, respiratory problems, asthma, sleep disturbances, stress, depression, ear infections, allergies, sore throats, insomnia.
As time moves forward, the acceptance of chiropractic practice in the medical community as a valid for of treatment for neuro-musculoskeletal conditions continues to increase. Chiropractic care is often the first line of recommendation for functional disorders of the entire musculoskeletal system from medical doctors.
Increasingly over the past few decades, the medical community has come to accept and recognize chiropractic care as a valid form of treatment for a variety of neuro-musculoskeletal conditions, and as a conservative treatment option for patients with lower back pain. Moreover, many medical doctors recognize a chiropractic diagnosis and accept it as the first line of treatment for functional disorders of the entire musculoskeletal system.
Articles on Chiropractic studies proving benefits of chiropractic care:
Your First Visit
Medical History
First things first, we will need some perspective.
Your history tells us where we should go with your treatment. The more information we have the better our diagnosis and in turn your outcome will be. All prior medical examinations, along with your vital signs, help us build a more complete picture of your health. We will ask you among other things:
- What are your pre-existing conditions?
- What drugs are you taking?
- What diagnoses, or examinations have you already had?
- Imaging or diagnostics
- X-rays
- MRIs
- CT scans
- What is your blood pressure?
- Weight?
- Imaging or diagnostics
- Do you have any allergies?
- Have you had any surgeries?
- What have you been up to in your daily life?
- Do you have an active lifestyle?
- What are you eating?
- What are your sleeping habits?
- What are the recent changes with your body?
Be ready to provide your medical history, which will be essential for preparing a course of treatment for you. Medical records, such as diagnostic test results, or imaging results, such as X-rays and MRIs, also will provide important information about your condition.
The Examination
We will inspect your body in a respectful, noninvasive manner consistent with the best practices of our industry.
The diagnostic procedures performed during your visit will vary from individual to individual based on your specific case but may include:
- Flexibility testing. Determining range of motion based on your ability to bend and stretch.
- Posture testing. The curvature of your spine while standing, sitting, and laying down.
- Strength testing – Looking for sign of muscle tension, pain, spasms and nerve damage by extension and contraction of muscular systems.
- Balance testing – Find the distance beyond the patients arm length that can be reached while keeping their feet planted.
- Reaction testing – Reflex hammer on the knee, biceps reflex, Achilles tendon reflex, triceps reflex, or brachioradialis reflex.
- Palpation – used to assess swelling or muscle tone, and assess tenderness through tissue deformation using pressure or stretching. Useful in determine painful areas and to qualify pain felt by patients, or to locate three-dimensional coordinates of anatomical landmarks to quantify some aspects of the palpated subject.
Depending on your outcomes more complex diagnostic tests may follow. These laboratory tests may include advanced imaging tools such as Magnetic resonance imaging, and X-ray computed tomography, in addition to blood work.
Post Examination Consultation
The consultation caters to your specific goals and needs as your situation dictates. You may be referred to other specialists or a plan for continued treatments may be necessary. Lifestyle choices will be discussed considering your nutrition, exercise, and health goals.

